News & Publications
Increasing Gonorrhea Rates Statewide
March 1, 2014
By David C. Hoak, M.D.
| County | 2011 | 2012 | County | 2011 | 2012 |
|---|---|---|---|---|---|
| Adams | 1 | 8 | Lewis | 6 | 12 |
| Asotin | 6 | 0 | Lincoln | 0 | 1 |
| Benton | 30 | 49 | Mason | 6 | 15 |
| Chelan | 8 | 10 | Okanogan | 8 | 5 |
| Clallam | 15 | 2 | Pacific | 2 | 3 |
| Clark | 159 | 151 | Pend Oreille | 0 | 4 |
| Columbia | 0 | 2 | Pierce | 424 | 657 |
| Cowlitz | 19 | 26 | San Juan | 1 | 4 |
| Douglas | 7 | 3 | Skagit | 16 | 22 |
| Ferry | 1 | 2 | Skamania | 4 | 1 |
| Franklin | 18 | 24 | Snohomish | 169 | 165 |
| Garfield | 0 | 1 | Spokane | 158 | 181 |
| Grant | 21 | 59 | Stevens | 2 | 1 |
| Grays Harbor | 12 | 5 | Thurston | 57 | 88 |
| Island | 6 | 19 | Wahkiakum | 0 | 0 |
| Jefferson | 3 | 1 | Walla Walla | 3 | 9 |
| King | 1,376 | 1,527 | Whatcom | 18 | 49 |
| Kitsap | 54 | 57 | Whitman | 11 | 26 |
| Kittitas | 9 | 8 | Yakima | 99 | 82 |
| Klickitat | 1 | 3 | Statewide | 2,730 | 3,282 |
Health officials across the Northwest are trying to figure out why they see a sizeable increase in the number of gonorrhea cases recently. Washington health officials announced last October that five counties were experiencing an outbreak of the infection. The Washington outbreaks occurred in Spokane, Benton, Yakima, Kitsap and Thurston counties. Overall, the state reported a 34% increase in gonorrhea cases in a year’s time.
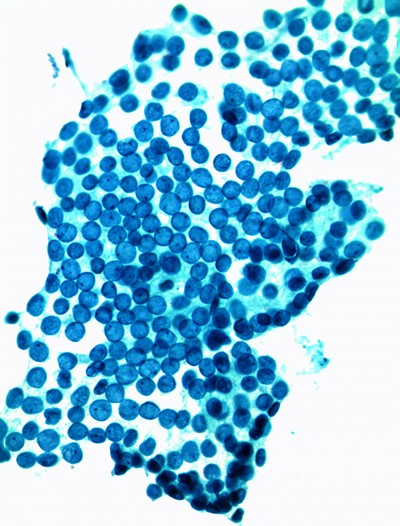
According to the Washington State Department of Health, gonorrhea is the second most commonly reported sexually transmitted disease in Washington after chlamydia. It is spread through unprotected sex with an infected partner. The infection often has no symptoms, particularly among women.
If symptoms are present, they may include discharge or painful urination. Serious long-term health issues can occur if the disease is not treated, including pelvic inflammatory disease, infertility and an increased likelihood of HIV transmission. In 2012 alone, 3,282 new cases of gonorrhea were reported in Washington state, which represents a sharp increase from the low of 1,880 cases reported in 1997.
Gonorrhea cases declined steeply both nationally and in Washington during the middle of the 1990s. Since 1997, gonorrhea incidence among Washington residents sharply increased through 2006. This pattern is consistent with trends
seen elsewhere on the west coast of the United States. The rate of new cases decreased steadily through 2009 perhaps in response to widespread implementation of improved treatment resulting in decreased transmission of the disease. The rate of gonorrhea has since sharply increased through 2012 to 48 cases of gonorrhea per 100,000 residents.
Historically in Washington, gonorrhea cases have been concentrated in urban areas. The state’s two largest urban counties, King and Pierce, had higher incidence rates than the overall state rate for the years 2010–2012 combined. A high incidence of gonorrhea among urban gay, bisexual and other men who have sex with men (MSM) contributes to the high rates of disease in these counties. Fourteen counties had too few cases for calculating reliable rates, and the remaining counties had incidence rates lower than the statewide average incidence rate of 48 cases per 100,000.
The number of gonorrhea cases reported among males is higher than among females. However, Gonorrhea cases in 2012 among males 15–19 years old was less than half that of females in the same age group, suggesting that younger men might be less likely to access screening and diagnostic services.
The Washington Health Department has asked health providers in the outbreak areas to increase STI screening of patients. The state offers expedited partner therapy, which allows sexual partners of people diagnosed with gonorrhea to automatically receive medication.
Rural and urban counties across eastern and western Washington have all reported a climb in cases. However, several counties have seen more dramatic upswings, including Spokane, Yakima, Thurston, Kitsap and Benton counties – which are at outbreak levels. Officials said rates have been increasing steadily since 2010, but experts are not sure why. The jump has occurred among men and women in most age groups, but young adults remain the most likely to be infected.
| YEAR | CASES | RATE |
|---|---|---|
| 1980 | 14,215 | 344.0 |
| 1981 | 13,204 | 312.2 |
| 1982 | 11,381 | 266.1 |
| 1983 | 9,895 | 229.7 |
| 1984 | 9,158 | 210.3 |
| 1985 | 10,073 | 228.1 |
| 1986 | 9,848 | 220.7 |
| 1987 | 8,909 | 196.8 |
| 1988 | 7,154 | 155.0 |
| 1989 | 6,369 | 134.7 |
| 1990 | 5,009 | 102.9 |
| 1991 | 4,441 | 88.4 |
| 1992 | 4,169 | 81.1 |
| 1993 | 3,740 | 71.0 |
| 1994 | 2,893 | 53.9 |
| 1995 | 2,765 | 50.5 |
| 1996 | 2,020 | 36.3 |
| 1997 | 1,955 | 34.5 |
| 1998 | 1,948 | 33.9 |
| 1999 | 2,132 | 36.6 |
| 2000 | 2,419 | 41.0 |
| 2001 | 2,991 | 50.1 |
| 2002 | 2,925 | 48.3 |
| 2003 | 2,754 | 44.9 |
| 2004 | 2,810 | 45.3 |
| 2005 | 3,738 | 59.3 |
| 2006 | 4,231 | 65.9 |
| 2007 | 3,646 | 55.9 |
| 2008 | 3,116 | 47.2 |
| 2009 | 2,268 | 34.0 |
| 2010 | 2,865 | 42.6 |
| 2011 | 2,730 | 40.3 |
| 2012 | 3,282 | 48.1 |
| * All rates are cases per 100,000 Note: Data prior to 2009 are based on year reported rather than year diagnosed. |
||
Gonorrhea is becoming increasingly resistant to the antibiotics that providers use to treat it.
Gonorrhea is one of the most common sexually transmitted diseases in the United States, where more than 800,000 gonorrhea infections are estimated to occur each year. Left untreated, gonorrhea can cause serious health problems, particularly for women, including chronic pelvic pain, life threatening ectopic pregnancy, and infertility. Gonorrhea infection also increases a person’s risk of contracting and transmitting HIV.
Health officials are on high alert for gonorrhea because it has a history of becoming resistant to treatments. Quinolone resistant N. gonorrhoeae strains are common in the United States and as of 2007, this group of antibiotics is no longer recommended for the treatment of gonorrhea. In 2011, 49% of samples from the Gonococcal Isolate Surveillance Project (GISP) collected in Seattle’s primary STI clinic from men with gonorrhea showed resistance to antibiotics formerly used to treat the disease. Overuse or incorrect use of antibiotics and gonorrhea’s ability to mutate rapidly in response to treatment are believed to be the main reasons the bacteria is becoming resistant to available treatments.
Currently, only the cephalosporin class of antibiotic is recommended for gonorrhea treatment. GISP project monitoring for patients with decreased susceptibility to these drugs is ongoing in Washington. Nationally, laboratory data suggest gonorrhea is becoming less susceptible to cefixime, the previously recommended oral medication used to effectively treat the disease. As a result, STI treatment guidelines now advise combination therapy that includes intramuscular ceftriaxone plus an oral drug. The possibility that reduced susceptibility may result in future treatment failure requires ongoing clinical vigilance to ensure patients are cured of gonorrhea infection.
Two new antibiotic regimens using existing drugs, injectable gentamicin in combination with oral azithromycin and oral gemifloxacin in combination with oral azithromycin, successfully treated gonorrhea infections in a clinical trial. The trial for these drugs was conducted by the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH). The study was conducted to identify new treatment options in the face of growing antibiotic resistance.
Researchers found 100% effectiveness of the injectable gentamicin/oral azithromycin combination in curing genital gonorrhea infections, and 99.5% effectiveness of the oral gemifloxacin/oral azithromycin combination. Both combinations cured 100% of infections of the throat and rectum. However, many trial participants reported adverse effects from the drugs, mostly gastrointestinal issues.
The CDC recommends only one first-line treatment regimen: injectable ceftriaxone, in combination with one of two other oral antibiotics, either azithromycin or doxycycline. This regimen remains highly effective in treating gonorrhea and results in limited side effects. However, providers may consider using the regimens studied in this trial as alternative options when ceftriaxone cannot be used, such as in the case of a severe allergy. The CDC is taking the findings of this trial into consideration for inclusion in future treatment guidelines.
It remains critical for people to take steps to protect themselves from gonorrhea infection. The surest way to prevent infection is not having sex. For those who are sexually active, consistent and correct condom use and limiting the number of sex partners can help reduce the risk of infection.