News & Publications
Cystic Thyroid Nodules (CTN) - Summary Points
January 5, 2012
By Felix Martinez Jr, M.D.
Cystic thyroid nodules (CTN) are very common and are frequently aspirated for cytology examination. In what follows, I attempt to summarize notes, key points, and my experience with cystic lesions.
CTNs
- Common
- 15-20% of solitary thyroid nodules are purely cystic
- 40% of thyroid nodules have at least a small cystic component
- Often recur after needle drainage
Etiology
- Common: hemorrhagic degeneration of hyperplastic regions of the thyroid parenchyma.
- Rare: hemorrhagic necrosis/cystic change of malignant thyroid neoplasm
Management of CTNs
- Controversial
- In the past, all CTNs considered benign and managed conservatively
- Currently, we still struggle with the possibility (admittedly low probability) of malignant cyst.
- Unfortunately, no clinical or pathologic criteria reliably distinguish between benign and malignant CTN.
General Diagnostic Approach
- Fine Needle Aspiration (FNA)
- Ultrasound-Guided FNA is especially useful for obtaining a sample of the solid portion of a thyroid cyst.
FNA Findings in a Pure Cyst

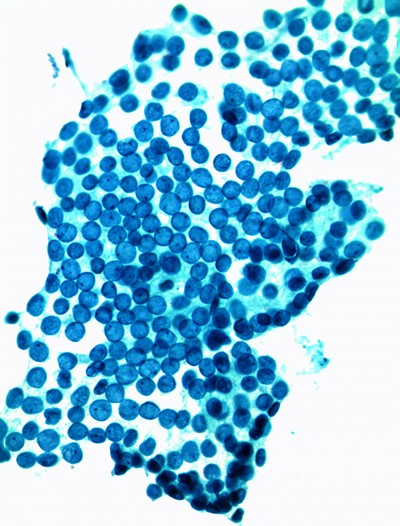
Figure 1. Cytology of Cyst Contents
“Cyst contents” Comprised of (in decreasing order of occurrence):
- proteinaceous debris
- foamy histocytes
- blood
- hemosiderin-laden macrophages
- multinucleated giant cells
- cholesterol crystals
Risk of Malignancy
- Low (4%) in purely cystic nodules
- Increases to 14% in:
✓ mixed solid cystic lesions
✓ cysts larger than 4 cm
✓ recurring cysts
Risk Factors for Possible Malignant CTN
- Large ( >3.5 cm) cyst size
- Bloody cystic fluid on first pass of FNA
- Recurrent cyst (incomplete cyst resolution)
- History of neck irradiation
False Negative (FN) Diagnosis
- FN = Missed Diagnosis
- FN in CTN varies in different studies, ranging from 1.5% to 11.5% (average 2-5%)
- Defined by thyroidectomy specimens having malignancy and occurring in patients with “benign” preceding cytology.

Cyst-lining cells with nuclear enlargement
False Positive (FP) Diagnosis in CTN
- Reparative changes can display marked cytologic atypia
- Repair: Fibroblasts, new blood vessels, damaged/regenerating thyroid follicles
- Reactive/reparative changes are a cause of FP results
- Cellular lining of a cyst often has repair
- Major differential diagnostic considerations are usually between cyst-lining cells with repair versus cystic papillary thyroid carcinoma.
Common Error in Technique During FNA
- A cause of false negative FNA of a cystic lesion is when a needle penetrates a cyst and cyst contents rapidly fill the aspirating needle (and/or the attached syringe), leaving little time to perform the important FNA in-and-out motion maneuvers.
- Sampling error, therefore, can occur when an aspirating needle remains stationary, thereby merely evacuating the cyst rather than sampling the tissue within or around a cystic nodule.
- In order to sample adequately and thoroughly, the aspirating needle needs to continually move in and out while the cyst is draining. This “sewing machine” motion is paramount to adequate collection, whether the target lesion is solid or cystic. Sampling a thyroid cyst is not be like drawing blood, where the needle remains stationary.

Benign atypia can have alarming appearance
Determination of “Adequacy” in FNA of CTN: Subjective and Controversial
- Most FNAs of CTNs are comprised of cyst fluid only with little, if any, associated epithelium to identify the type of cyst.
- No clinical study unequivocally supports any specific cellularity/ number of follicles as applicable in all cases.
- No consensus regarding minimum number of FNA passes required to obtain “adequate” sample.
- Incyte’s Approach for Cystic Lesions: Proficient collection combined with excellent slide preparation, processing, staining, and cytopathologic interpretation.
Bethesda System for Reporting Thyroid Cytopathology (BSRTC)
- Recommends that all thyroid FNA reports have a “general diagnostic category” in the first diagnostic line (Benign, Indeterminant, Atypical, Suspicious, Malignant) followed by a description of findings
- BSRTC FNA Criteria for Adequacy: “minimum of six groups of well visualized follicular cells, with at least 10 cells per group.”

Figure 3. Cystic Papillary Thyroid Carcinoma
Problems With the Terms “Non-Diagnostic” and “Inadequate/Unsatisfactory”
- Historically, these terms were used interchangeably by some interpreting pathologists, with others using the terms to mean different things, a problem that continues today.
- By National Cancer Institute (NCI) criteria, the terms “non-diagnostic” and “unsatisfactory” were recommended to describe an inadequate or insufficient sample.
- In CTN reporting, Bethesda criteria terminology uses “non-diagnostic” to mean “repeat collection needed.”
FNA CTNs Lacking an Epithelial Component
- Hard to Interpret
- Low risk for cystic malignancy exists
- Formerly deemed “less than optimal,” diagnostic terminology unsatisfying for all (clinician, pathologist, patient).
- According to BSRTC, cyst fluid having fewer than six groups of ten, well-preserved, benign follicular cells is considered “non-diagnostic/unsatisfactory”
Malignancy In a CTN
- Of all the thyroid neoplasms, Papillary Thyroid Carcinoma (PTC) is most commonly cystic.
- When a FNA diagnosis of “cyst” occurs in a clinical setting suspicious for malignancy, false-negative FNA results are possible and the patient should be followed closely.

Figure 2. Cystic Papillary Thyroid Carcinoma Nodule
Limitations of FNA of CTNs
- FNA has a poor track record in diagnosis of any cystic lesion at any anatomic site. Thus, thyroid cysts are a common cause of false-negative diagnosis
- Greater risk of sampling error
- Cyst may collapse, thereby becoming less echogenic on ultrasound, thereby possibly being undersampled in subsequent passes due to loss of visualization of the lesion.
- Cystic papillary thyroid carcinoma (PTC) may yield few to none malignant cells on any given FNA pass. (see figure 2)
Sensitivity and Specificity of FNA of Thyroid Nodules
| nodule type | sensitivity | specificity |
| solid | 95% | 75% |
| cystic | 88% | 52% |
- Cystic lesions are as likely as solid lesions to harbor malignancy.
- Likelihood of malignancy within a cyst cannot be predicted from the cysts clinical or imaging characteristics, or the patient’s demography.
- Although FNA is the best predictor of malignancy in either cystic or solid lesions, it is less reliable when a thyroid target lesion is fluid-filled rather than solid.
Predictive Value of a Negative Result (PVNR) in FNA of CTN
Fortunately, given all of the limitations discussed, the PVNR is high because:
- Nearly all of cystic thyroid nodules are benign.
- The prevalence of malignant thyroid nodules is low.
- The prevalence of cystic papillary thyroid carcinoma is low.
- Malignant cysts are mostly papillary carcinoma.
Incyte Diagnostics Approach to CTNs
- Acknowledge the difficulties (many)
- Understand the risk (low)
- Promote clinician education regarding #1 and #2 above
- Encourage good FNA technique and effective sampling of CTNs.
- Pathology report: describe what is present in the sample using terminology understood by our providers.
- Minimize repeat procedures for patients having low probability of malignancy.
- Encourage repeat sampling in patients having paucicellular samples, large (>3.5 cm) cystic lesions, a history of irradiation, or clinical/imaging findings suspicious for malignancy and/or negative cytology findings discordant with clinical picture.
References
Feld S, 1996 AACE Clinical Practice Guidelines for the Diagnosis and Management of Thyroid Nodules, Endocr Pract, Vol 2 No. 1.
Cooper D, 2009 Revised American Thyroid Assoc Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer, THYROID, Vol 19, No. 11.
Bennedbaek FN, Hegedus L 2003 Treatment of recurrent thyroid cysts with ethanol: a randomized double-blind controlled trial. J Clin Endocrinol Metab 88:5773-5777.
Valcavi R, Frasoldati A 2004 Ultrasound-guided percutaneous ethanol injection therapy in thyroid cystic nodules. Endocr Pract 10:269-275.
Antonelli A, Campatelli A 1994 Comparison between ethanol sclerotherapy and emptying with injection of saline in treatment of thyroid cysts. Clin Investig 72:971-974.
Verde G, Papini E 1994 Ultrasound-guided percutaneous ethanol injection in the treatment of cystic thyroid nodules. Clin Endocrinol (Oxf) 41:719-724.