News & Publications
ASC-US vs. ASC-H? What is the difference?
October 17, 2011
By Felix Martinez Jr, M.D.

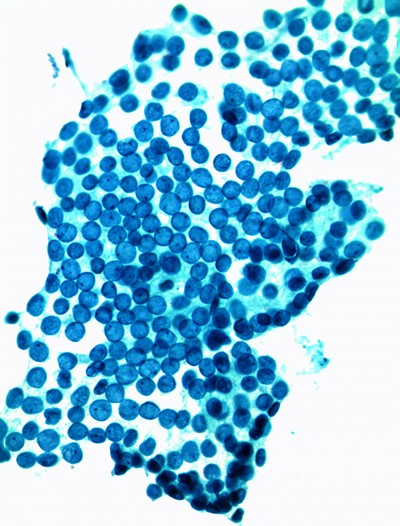
Figure 1
History
The current nomenclature now used to report Pap findings in the United States began with a meeting of a small group of experts in December of 1988 in Bethesda, Maryland. The results of this conference were termed the 1988 Bethesda System (TBS). Of all the TBS changes that were introduced by this conference, none was as problematic and controversial as “atypical squamous cells of undetermined significance” or “ASC-US”.
The silver lining of the black cloud created by ASC-US was the initiation of a large clinical trial, the ASC-US/LSIL Triage Study (ALTS), which was sponsored by the NCI and conducted under the auspices of the American Society for Colposcopy and Cervical Pathology (ASCCP). ALTS provided data for the development of evidence-based guidelines for management of women with abnormal results reported using TBS terminology.
In the end , an algorithmic management approach was developed, with examples seen in Figures 2 & 3 (on page 3). It was a landmark event that an ancillary test for human papilloma virus (HPV) was employed to determine which women should go to colposcopy after ASC-US Pap findings.
Atypical Squamous Cells (ASC)
Atypical squamous cells represent cellular abnormalities more marked than simple reactive changes, but which do not meet the criteria for squamous intraepithelial neoplasia (SIL). These cells are not of typical appearance and are, therefore, atypical. (See Figure 1).
Categories of ASC
The Pap diagnosis of Atypical Squamous Cells (ASC) is the most common abnormal finding during cervical cancer screening and is reported in about 5 percent of all cervical screening tests.

Illustration 1, ASC-US
There are two subtypes of ASC:
- Atypical Squamous Cells of Undetermined Significance (ASC-US)
- Atypical Squamous Cells, Cannot Rule Out High Grade Squamous Intra-epithelial Lesion (ASC-H). For a diagnosis of ASC-US, a Pap smear has to have a specific type of abnormal cells (see Illustration 1).
Most nuclear enlargement in Pap tests is due to reactive change, and reactive changes and LSIL must be excluded by the pathologist when an ASC-US diagnosis is provided. At Incyte Diagnostics, our ASC-US rate is 3.7%. ASC-US results initiate reflex HPV testing, with positive HR HPV test results prompting colposcopic examination. ASC-US is the most common of the ASC diagnoses.

Illustration 2, ASC-H
ASC-H Requires Colposcopy
Since a high grade squamous intraepithelial lesion (HSIL) cannot be excluded in ASC-H, triage directly to colposcopy is recommended by the ASCCP for ASCH diagnosis. ASC-H is rare in our laboratory (0.2%). ASC-H cells are depicted in Illustration 2.
For a diagnosis of ASC-H, the cytopathologist must first exclude moderate/severe cervical intraepithelial neoplasia or carcinoma in-situ (CIN3/HSIL). In some cases, women having ASC-H findings may harbor HSIL or invasive cervical cancer in their follow up.
Of all women with HSIL results, 2% or less have invasive cervical cancer at the time of diagnosis. About 20% can however, progress to have invasive cervical cancer if not treated or followed appropriately. Relative risk for ASC-H Pap diagnosis is certainly less than 20%, but HSIL must first be excluded by colposcopy and biopsy after ASC-H findings. If no colposcopic lesion is visible in follow up of ASC-H, vigorous ECC should be undertaken.

Figure 2

Figure 3
At this time, there is often confusion (and even controversy) among healthcare providers regarding the proper evaluation and management of ASC, especially ASC-H.
The ASCCP 2006 consensus guidelines for the evaluation of women with cervical cytology (ASC-US and ASC-H) are provided (Figures 2 & 3).
Summary
Since 1988, the diagnosis of Atypical Squamous Cells has evolved from a poorly-defined, wastebasket category of diagnosis into an evidence-based triage test which employs a very sensitive risk stratification assay (i.e., the HPV test) to determine which patients need colposcopy. Current algorithms have helped greatly to standardize clinical management of patients with ASC abnormalities.